DEFINITION
- Apraxia – derived from Greek word, praxis, meaning to do or action
- An acquired disorder of skilled purposeful movement
- purposeful important b/c may do automatically (e.g., can spontaneously brush crumbs off lap but can’t do so on command or intentionally)
- Syndrome of higher motor dysfx
- distinct from paresis in same way aphasia distinct from dysarthria
- analogous to agnosia, a syndrome of higher sensory dysfx
- NOT caused by paresis, abnormal tone or posture, akinesia, ataxia, sensory loss, inattention, poor comprehension or other cognitive problems (i.e., primary motor skills and comprehension ok)
- In practice, term sometimes used as shorthand for ideomotor apraxia, most common type
HISTORY
- Term introduced in 1870 by Steinthal, but prior to 1890 much confusion and not clearly differentiated from aphasia and agnosia
- In 1900, Hugo Liepmann (one of Wernicke’s students) clearly established apraxia as distinct disorder; later provided classification of subtypes and theory of normal and abnormal actions (praxis)
- Much debate since about definitions, etiology, etc.
LIEPMAN’S NEUROANATOMICAL MODEL
- suggested that the left parietal area is critical for control of complex movement; mediated by the left frontal lobe and area 4 for the right side of the body; disruption anywhere in this system would produce right-sided apraxia
- control of the left limbs was proposed to be mediated through cnxns from the left parietal area to the left frontal cortex and then to the right frontal cortex (via CC)
- problems with this theory include:
- does not recognize the involvement of the basal ganglia and thalamus in movement
- although it is assumed that the posterior parietal and prefrontal regions are the primary regions involved in apraxia, patients w/circumscribed cortical lesions do not typically demonstrate chronic abnormalities on standard clinical tests of apraxia (emphasizes basal ganglia and thalamus’ role in apraxia)
MAIN SUBTYPES
3 Classic types defined by Leipmann
Limb-Kinetic Apraxia (aka, melokinetic or innervatory apraxia)
Leipman defined melokinetic as the loss of kinetic memories for a single limb; related to small lesions in motor cortex which are insufficient to produce paresis
- Movements appropriate to intended action, but movements are clumsy, unskilled, or imprecise
- Affects fine-motor movements, especially finger movements (gross motor ok)
- More obvious when testing distal movements, and is especially evident when making rapid movements (like finger tapping)
- Defect is unilateral, opposite to involved hemisphere
- Least frequently dx, reflecting uncertainty about how differs from mild paresis or ataxia
- Current definitions might consider this apraxia more of an ataxia
Testing
- Simple manual acts troublesome (e.g., playing cards, picking up coin from table, buttoning shirt)
- Problems on grooved pegboard, finger-tapping speed, etc.
Lesion Site
- Limited lesions of contralateral premotor area or subjacent white matter
Ideomotor Apraxia
(Leipmann first called motor apraxia and then ideokinetic apraxia)
- Defective execution of individual components of action
- comprehension ok, motor system intact, and activity can be performed spontaneously
- Separation exists between idea of an act and its performance (i.e., “disconnection b/t idea of movement from kinetic memory images)
- See w/ both transitive (using tool/instrument) and intransitive (not involving tools/objects such as wave good-bye, cough) commands, although transitive typically more impaired
- Refers to single action, not a sequential motor performance
- Errors can improve upon imitation
- Can be seen in oral (buccofacial), limb, or axial musculature
- In contrast to limb-kinetic, typically see bilateral deficits (although can be unilateral)
Testing
- Most notable when asked to pantomime actions to verbal commands
- First test by “Show me….”
- Then see if improves upon imitation
- Then see if improves w/ use of actual object
- Buccofacial (i.e., oral apraxia) ~ first described by Hughlings Jackson
- Gesture: Kiss the air, repeat “Pa”
- Imagined: Pretend to blow out a match, suck w/ a straw, cough
- Real: blow out match, drink water thru straw
- Common among Broca’s aphasics
- Limb
- Gesture: Salute, stop traffic, wave good-bye
- Imagined: Pretend to use a comb, to write, use a screwdriver
- Real: comb hair, write w/ pencil or pen
- Axial
- eyes look up; close your eyes; neck: bend head down; trunk: stand, kneel, walk backwards
- may be mediated by different pathways since often preserved even in severe apraxia
Errors
- Failure to generate response
- Spatial: correct core movement, but limb movement thru space incorrect (e.g., sawing horizontally rather than vertically)
- Perseveration: e.g., after blowing match, repeats for sucking straw
- Verbalization is produced instead of action (saying “cough,” instead of coughing)
- Use body part as part of object (using hand for comb)
- Sequential: sequencing errors (demonstrating key use by rotating wrist, then extend arm)
- Timing: Failure to coordinate speed w/ spatial aspects of gesture
Lesion site
- Left-hemisphere dominance for praxis
- Can occur w/ lesions anywhere w/in perisylvian region
- Occurs after damage to one or more areas (Ansher and Benson, 1993)
- Lesion to L par lobe can damage arcuate fasciculus, which interrupts flow of info anteriorly and prevents motor system from receiving direction to act (conduction aphasia often seen)
- Large lesion to L premotor area interferes w/ motor execution (often seen w/ nonfluent aphasia and hemiparesis)
- Lesion to anterior corpus callosum leads to apraxia; only seen w/ left hand (no aphasia)
Ideational Apraxia
- Failure to perform a sequential motor movement, though each individual component can be performed in isolation (e.g., completed in the wrong order or perseverate on single step)
- Fail at complex task because of faulty overall plan or “idea”
- Component skills ok, but include wrong ones or in wrong order when completing sequence
- In contrast to limb-kinetic, see bilateral deficits
- Lots of conceptual confusion in definition of ideational apraxia; practical utility may be limited
Testing
- Have pt perform series of component actions in correct order
- Fold letter, insert in envelope, seal it, apply postage
- Light candle: give box of matches and candle
Lesion site
- Localization unsettled, but seen w/ both:
- damage to left parietal lobe (large lesion)
- most commonly occurs with diffuse cortical involvement from dementia
- May represent primary disturbance of attention or executive fxs (Weintraub)
MECHANISMS UNDERLYING APRAXIA
Over the years, two general hypotheses proposed
Disconnection Hypothesis
- First proposed by Leipmann and then vigorously defended by Geschwind
- Disconnection of critical left cortical areas from zones of execution (see above under ideomotor); inability to elicit correct motor sequences in response to language
- Discnxn b/t language areas and visuokinesthetic engrams
- fibers either cross from (1) Wernicke’s area to the contralateral association area or (2) from the left premotor area to the premotor area on the right
- lesions that destroy the left premotor cortex are often associated w/right hemiplegia, but if the patients were not hemiparetic, they would probably be apraxic on the right
- lesions w/c disconnect the posterior language area from the motor association cortex (in the arcuate fasciculus) cause patients to be able to understand directions but not perform them
- Does NOT explain why pts w/ such lesions can’t imitate gestures
Representational (or Praxicon) Hypothesis
- Heilman argues for existence of “visuo-kinesthetic engrams” or “praxicons” in the inferior par. lobe
- Based on idea that nervous system learns and stores skilled movements
- Kimura has argued that this knowledge is stored in the dominant parietal lobe
- A disconnection b/t the area that stores this info and the premotor/motor areas will result in poor implementation of skilled movements
- When first learning skilled movement, basal ganglia and cerebellum play role, but later memories involve cortical representation – praxis represents motor equivalent of remote memories
- Supported by fact that some apraxic pts lose ability to form movements, as well as ability to recognize correct movements in others
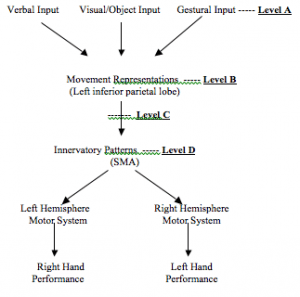
IDEOMOTOR APRAXIA MODEL
Model depicting possible impairments in ideomotor apraxia
- Level B Lesion: Can’t recognize gestures because damage to representations of learned, skilled movements; gesture discrimination problem
- Level C Lesion: Bilateral ideomotor apraxia but can comprehend and discriminate gestures; movement memories not destroyed, just can’t interact w/ anterior areas responsible for motor implementation
- Level D Lesion: Bilateral ideomotor apraxia but can comprehend and discriminate gestures; innervatory patterns can’t gain access to motor area
DIFFERENTIAL DIAGNOSTIC ISSUES
- Disorders of basal ganglia and cerebellum may be associated w/ nonapraxic movement disorders such as postural change, tone, tremor, etc.
- Aphasia
- Many apraxic patients are also aphasic (b/c of lesions near or overlapping speech centers), so must be distinguished
- If pt performs poorly when required to indicate with limb, but performs okay when required to provide a yes/no answer, they may be apraxic
- tend to occur in clusters of disabilities that share a common anatomical pattern
- g., apraxias of impaired ability to perform skilled tasks on command or imitatively or to use objects are commonly associated with language deficits (b/c of lesions near or overlapping speech centers)
- g., facial apraxia and deficits in expressive speech (Broca’s aphasia); anatomical regions for verbal expression and facial movement are close
- anosognosia – frequently have right-hemiparesis and may attribute clumsiness to the use of their non-dominant hand
TERMINOLOGY CLARIFICATION
Many neurobehavioral syndromes with some motor dysfx have been termed “apraxia” but likely not really apraxia as traditionally defined
Constructional apraxia
(Kleist; also associated with Hecaen)
- Problem with drawing, assembling, or building
- Bears no relation to Liepmann’s definition of apraxia, thus “visuoconstructive impairment” might be better term
- Can be tested by paper and pencil (copy drawing; draw house, clock, etc), three-dimensional construction
- Traditionally thought to be caused by parietal lesions (either left or right)
Dressing apraxia
- difficulty with dressing (follows rt hemi lesions)
- Also bears little relation to original apraxia definitions (e.g., no dissociation b/t voluntary-automatic and performance on command )
- Perhaps most frequent in dementia or confusional states
- Caused by any number of lesions, including left-sided neglect, Balint’s syndrome (simultanagnosia or optic ataxia)
- NOT seen in isolation
Ocular apraxia
Oculomotor apraxia or psychic paralysis of gaze
- Inability to perform purposeful ocular movements
- component of Balint’s syndrome
- deficit in visual scanning; inability to shift gaze at will toward new visual stimuli and inability to maintain fixation on an object
- Almost always accompanied by either optic ataxia or visual disorientation
Optic apraxia/Optic Ataxia
- Apraxia of ocular searching movements affecting visually guided hand movement
- Usually results from bilateral posterior parietal lesions
- Sxs same for optic apraxia/optic ataxia – different terms vary in emphasis on underlying neurobehavioral deficits that accounts for phenomenon
- Seen in Balint’s syndrome
Gait apraxia
- d/o of gait seen in diseases affecting frontal lobe
- First and most prominent sx of Normal Pressure Hydrocephalus
- Seen when pts fail to alternate leg movements, don’t shift weight forward, pick up same leg twice in row; foot can be “magnetized” to floor
- Most pronounced when starting to walk
- Stepping reflex preserved so might step over obstacle spontaneously
Verbal apraxia (aphemia)
- used by speech pathologists to describe pxs w/ speech fluency or dysarthria
Apraxia of speech
- an articulation d/o resulting from brain damage
- impairment in capacity to program positioning of speech musculature and sequencing of muscle mvmts
- not a language/aphasia problem
- in contrast to dysarthria, practice worsens condition
- inconsistent articulation errors; pts sounds like they are struggling to articulate words
Callosal apraxia (aka, unilateral apraxia)
- form of ideomotor apraxia ass’d w/ difficulty in executing motor sequencing tasks of the left hand following lesions of the CC
- thought to result from disconnection of the visuokinetic motor engrams of the left hemisphere from the motor area of the right
- seen in lesions affecting fibers passing through the anterior CC
Conceptual Apraxia
- an inability to perform limb movements on command resulting from impairment in linking the meaning or intent of an action to movement plan
- movements are well performed but inaccurate in content
Frontal apraxia
- An inability to perform routine actions because of temporal or sequential disorganization
- Verbal mediation does not improve performance
Links between goal of action and specific acts that must be “assembled” to serve goal become destabilized and action sequence becomes a series of isolated fragments